Leishmaniasis is a serious and potentially fatal disease caused by a group of microscopic parasites called Leishmania. These parasites are transmitted to humans and animals by the bite of infected sandflies, which are tiny insects that live in tropical and subtropical regions of the world. Leishmaniasis can affect the skin, mucous membranes, and internal organs, depending on the type and species of the parasite. In this article, we will explain the causes, symptoms, diagnosis, treatment, prevention, and control of leishmaniasis and risk factors of this disease.
Causes of Leishmaniasis
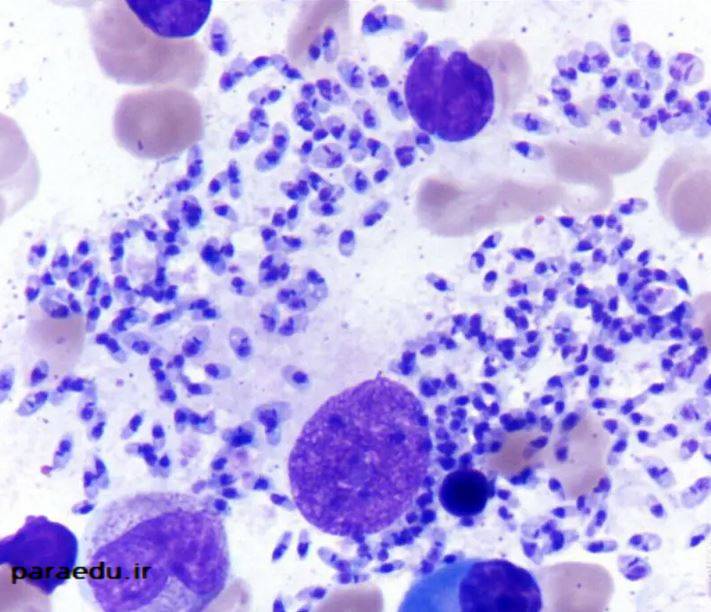
Leishmaniasis is caused by more than 20 species of Leishmania parasites, which belong to the group of protozoa, or one-celled organisms. These parasites have two main forms: the amastigote and the promastigote. The amastigote is the form that lives and multiplies inside the cells of the vertebrate host, usually macrophages or monocytes. The promastigote is the form that lives and develops in the gut of the sand fly, which is the insect vector that transmits Leishmania between vertebrate hosts. The promastigote has a flagellum, which is a whip-like appendage that helps it swim and attach to the sand fly’s mouthparts.
The transmission cycle of Leishmania parasites involves two hosts: a vertebrate host (such as a human or an animal) and an invertebrate host (the sand fly). The cycle is as follows:
- A female sandfly becomes infected by biting an infected vertebrate host and ingesting the amastigotes along with the blood.
- The amastigotes transform into promastigotes in the sand fly’s gut and multiply there.
- The promastigotes migrate to the sand fly’s mouthparts and are ready to infect another vertebrate host.
- The sandfly bites another vertebrate host and injects the promastigotes along with its saliva.
- The promastigotes enter the host’s cells and transform into amastigotes, which start to multiply and cause the disease.
Sand flies
The sand flies that carry Leishmania parasites are usually active during twilight, evening, and night-time hours (from dusk to dawn). They are attracted by the heat, carbon dioxide, and movement of their hosts. They prefer to bite the exposed parts of the body, such as the face, arms, and legs. The sand flies are very small (2 to 3 millimeters long) and their bite is often painless, so many people may not notice that they have been bitten.

Species of Leishmania parasites and sandfly
The species of Leishmania parasites and the sand flies that transmit them vary depending on the geographic region and the type of leishmaniasis. Some of the most common species of Leishmania and their associated sand flies are:
- Leishmania donovani and Leishmania infantum, which cause visceral leishmaniasis, are transmitted by Phlebotomus sand flies in the Old World (Africa, Asia, and Europe) and by Lutzomyia sand flies in the New World (the Americas).
- Leishmania tropica and Leishmania major, which cause cutaneous leishmaniasis, are transmitted by Phlebotomus sand flies in the Old World.
- Leishmania braziliensis and Leishmania mexicana, which cause cutaneous and mucocutaneous leishmaniasis, are transmitted by Lutzomyia sand flies in the New World.
In some areas where leishmaniasis is found, infected people are not needed to maintain the transmission cycle of the parasite in nature; infected animals (such as rodents or dogs), along with sand flies, maintain the cycle. This type of transmission is called zoonotic. However, in some parts of the world, infected people are needed to maintain the cycle; this type of transmission (human—sand fly—human) is called anthroponotic. In areas with anthroponotic transmission, effective treatment of individual patients can help control the spread of the parasite.
Symptoms of Leishmaniasis
Leishmaniasis can manifest in three main forms: visceral, cutaneous, and mucocutaneous. The symptoms of each form depend on the type and species of the parasite, the immune status of the host, and other factors. The incubation period, or the time between the sand fly bite and the appearance of symptoms, can range from a few days to several months or even years.
Visceral Leishmaniasis
Visceral leishmaniasis (VL), also known as kala-azar, is the most serious and potentially fatal form of leishmaniasis. It affects the internal organs, such as the spleen, liver, and bone marrow, and can cause severe complications, such as bleeding, infections, and organ failure. VL is characterized by the following symptoms:
• Irregular bouts of fever, which may last for weeks or months.
• Weight loss and loss of appetite.
• Enlargement of the spleen and liver, which can be felt as a mass in the abdomen.
• Anemia, which is a low level of red blood cells that carry oxygen in the blood.
• Leukopenia, which is a low level of white blood cells that fight infections.
• Thrombocytopenia, which is a low level of platelets that help blood clotting.
• Darkening of the skin, especially on the face, hands, feet, and abdomen, which gives the disease its name kala-azar, meaning “black fever” in Hindi.
VL is fatal if left untreated in over 95% of cases. The mortality rate can be as high as 100% within two years of infection. Even with treatment, some patients may relapse or develop a condition called post-kala-azar dermal leishmaniasis (PKDL), which is a skin rash that occurs after the treatment of VL. PKDL can serve as a reservoir for the parasite and contribute to the transmission of VL.

Cutaneous Leishmaniasis
Cutaneous leishmaniasis (CL) is the most common form of leishmaniasis and causes skin lesions, mainly ulcers, on the exposed parts of the body. CL is usually not life-threatening, but it can leave permanent scars and cause serious disability or stigma. CL is characterized by the following symptoms:
- A small red bump (papule) at the site of the sand fly bite, which may appear a few days or weeks after the bite.
- The papule enlarges and develops into a raised sore (nodule) that may be painless or painful, dry or moist, and covered with a crust or a scab.
- The nodule breaks down and forms an open ulcer that may have a raised border and a depressed center. The ulcer may be single or multiple, and may vary in size and shape. The ulcer may be infected with bacteria or fungi and produce pus or discharge.
- The ulcer may heal spontaneously after a few months or years, or persist for a long time. The healing process may leave a depressed scar that may be disfiguring or impair the function of the affected body part.
In some cases, CL may spread to other parts of the skin or the mucous membranes of the nose, mouth, and throat. This form of CL is called diffuse cutaneous leishmaniasis (DCL) or mucocutaneous leishmaniasis (MCL), respectively. DCL and MCL are more difficult to treat and can cause severe damage to the tissues and organs involved.

Mucocutaneous Leishmaniasis
Mucocutaneous leishmaniasis (MCL) is a rare form of leishmaniasis that affects the mucous membranes of the nose, mouth, and throat. MCL is caused by the same parasites that cause CL, but it can occur several months or years after the skin ulcers heal. MCL is characterized by the following symptoms:
- Ulcers or sores in the nose, mouth, or throat that may bleed or produce discharge.
- Swelling or inflammation of the nose, lips, gums, tongue, or palate.
- Difficulty in breathing, swallowing, or speaking.
- Partial or total destruction of the nasal septum, the cartilage that separates the nostrils.
- Loss of the nose, lips, or parts of the face due to tissue erosion and necrosis.
MCL does not heal on its own and always requires treatment. If left untreated, MCL can lead to severe disfigurement, disability, and social stigma.

Diagnosis of Leishmaniasis
The diagnosis of leishmaniasis is based on the clinical signs and symptoms, the history of exposure to sand flies or endemic areas, and the laboratory tests. The laboratory tests can confirm the presence of the parasite or its DNA, antibodies, or antigens in the blood, tissue, or other body fluids of the patient. The laboratory tests can also identify the species of the parasite, which is important for choosing the appropriate treatment and predicting the outcome of the disease. Some of the laboratory tests used for the diagnosis of leishmaniasis are:
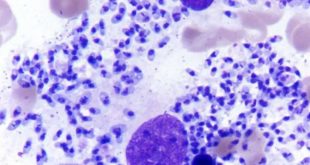
- Microscopy: This test involves examining a smear or a biopsy of the skin, mucous membrane, or bone marrow under a microscope to look for the parasite or its forms. The smear or the biopsy can be stained with special dyes to enhance the visibility of the parasite. Microscopy is a simple, fast,
and cheap method, but it has a low sensitivity and specificity, meaning that it may miss some cases or give false positive results. - Culture: This test involves growing the parasite in a special medium, such as a liquid or a solid agar, from a sample of the skin, mucous membrane, or bone marrow. Culture is a more sensitive and specific method than microscopy, but it takes longer (up to four weeks) and requires more expertise and equipment.
- Molecular tests: These tests involve detecting the DNA or RNA of the parasite in a sample of the blood, tissue, or other body fluids using techniques such as polymerase chain reaction (PCR) or loop-mediated isothermal amplification (LAMP). Molecular tests are very sensitive and specific, and can also identify the species of the parasite. However, they are expensive and require sophisticated laboratory facilities and trained personnel.
- Serological tests: These tests involve detecting the antibodies or antigens of the parasite in the blood or other body fluids using techniques such as enzyme-linked immunosorbent assay (ELISA) or rapid diagnostic tests (RDTs). Serological tests are easy to perform and can give results within minutes or hours. However, they have some limitations, such as cross-reactivity with other infections, low sensitivity in early or late stages of the disease, and difficulty in distinguishing between current and past infections.
- Immunological tests: These tests involve measuring the immune response of the patient to the parasite using techniques such as the leishmanin skin test (LST) or the interferon-gamma release assay (IGRA). Immunological tests can indicate the exposure or the resistance of the patient to the parasite, but they cannot confirm the diagnosis or the species of the parasite. They are also influenced by the immune status of the patient and the type of leishmaniasis.
The choice of the laboratory test depends on the availability, cost, accuracy, and feasibility of the test in the setting where the patient is diagnosed and treated. Sometimes, more than one test may be needed to confirm the diagnosis or to monitor the response to the treatment.
Treatment of Leishmaniasis
The treatment of leishmaniasis depends on several factors, such as the type and species of the parasite, the form and severity of the disease, the immune status and the age of the patient, the availability and cost of the drugs, and the potential side effects and drug resistance. The treatment should be individualized and guided by a health care provider with experience in managing leishmaniasis. The treatment options for leishmaniasis include the following:
- Antimonial compounds: These are the mainstay of therapy for all forms of leishmaniasis. They are given by intramuscular or intravenous injection for 20 to 28 days. The most commonly used antimonial compound is sodium stibogluconate. The main side effects of antimonial compounds are cardiac, hepatic, and renal toxicity. Antimonial compounds are not recommended for pregnant women, children under 2 years of age, and patients with pre-existing cardiac, hepatic, or renal disease. Antimonial resistance is a growing problem in some regions, especially in India and Sudan.
- Amphotericin B: This is an antifungal drug that has activity against Leishmania parasites. It is given by intravenous infusion for 10 to 20 days. The main side effects of amphotericin B are infusion-related reactions, such as fever, chills, headache, and nausea, and nephrotoxicity, which can lead to kidney failure. Amphotericin B is effective against antimonial-resistant leishmaniasis. A liposomal formulation of amphotericin B, which has fewer side effects and shorter duration of treatment, is available but more expensive.
- Pentamidine: This is an antiprotozoal drug that is used for the treatment of visceral leishmaniasis caused by Leishmania donovani in India and Africa. It is given by intramuscular injection for 14 to 21 days. The main side effects of pentamidine are hypoglycemia, which can cause low blood sugar levels, and pancreatitis, which can cause inflammation of the pancreas. Pentamidine is not effective against cutaneous or mucocutaneous leishmaniasis.
- Paromomycin: This is an aminoglycoside antibiotic that has activity against Leishmania parasites. It can be given by intramuscular injection for 21 days for the treatment of visceral leishmaniasis, or by topical application for 20 days for the treatment of cutaneous leishmaniasis. The main side effects of paromomycin are ototoxicity, which can cause hearing loss, and nephrotoxicity, which can cause kidney damage. Paromomycin is not effective against mucocutaneous leishmaniasis.
- Miltefosine: This is an oral drug that was originally developed for the treatment of cancer, but has shown efficacy against Leishmania parasites. It can be given for 28 days for the treatment of visceral or cutaneous leishmaniasis, or for 12 weeks for the treatment of mucocutaneous leishmaniasis. The main side effects of miltefosine are gastrointestinal disturbances, such as nausea, vomiting, and diarrhea, and teratogenicity, which can cause birth defects. Miltefosine is contraindicated for pregnant or breastfeeding women, and women of childbearing age should use effective contraception during and for 3 months after the treatment.
- Other drugs: Some other drugs that have been used for the treatment of leishmaniasis in some cases or in combination with other drugs include allopurinol, ketoconazole, itraconazole, fluconazole, and imiquimod. However, these drugs have limited evidence of efficacy and safety, and are not widely available or affordable.
Prevention of Leishmaniasis
There is no vaccine or prophylactic drug available for the prevention of leishmaniasis. The best way to prevent leishmaniasis is to avoid or reduce the exposure to sand fly bites, especially in endemic areas. The preventive measures for leishmaniasis include the following:
- Personal protection: This involves wearing long-sleeved shirts, long pants, socks, and shoes, and applying insect repellents containing DEET or other active ingredients to the exposed skin and clothing. The repellents should be reapplied according to the instructions on the label. The personal protection should be especially practiced from dusk to dawn, when the sand flies are most active.
- Environmental control: This involves using insecticide-treated bed nets, curtains, and screens, and spraying insecticides in the living and sleeping areas. The insecticides should be chosen according to the local sand fly species and resistance patterns. The environmental control should be implemented in coordination with the local health authorities and communities.
- Vector control: This involves reducing the breeding and resting sites of the sand flies, such as cracks and crevices in walls, animal burrows, and piles of rubbish or vegetation. The vector control should be based on the ecological and behavioral characteristics of the local sand fly species and involve the participation of the local population.
- Animal reservoir control: This involves identifying and treating the animal hosts of the Leishmania parasites, such as dogs, rodents, or other wild animals. The animal reservoir control should be done in collaboration with the veterinary services and the wildlife authorities. The methods of animal reservoir control include culling, vaccination, treatment, and collar impregnation with insecticides.
- Case detection and treatment: This involves finding and treating the human cases of leishmaniasis, especially the visceral and mucocutaneous forms, which can serve as sources of infection for the sand flies. The case detection and treatment should be done by trained health workers and with appropriate diagnostic and therapeutic tools. The case detection and treatment can reduce the morbidity and mortality of leishmaniasis and interrupt the transmission cycle of the parasite.

 انگل شناسی پزشکی Medical Parasitology
انگل شناسی پزشکی Medical Parasitology